October is Breast Cancer Awareness Month, a global moment to focus on prevention, early detection, and the incredible strides in treatment. While the successful journey from diagnosis to remission deserves celebration, the reality for many survivors includes a challenging, often overlooked condition: lymphedema.
It’s a complication that can significantly impact daily life, turning the “all clear” into a new, complex battle. This month, let’s look past the main event and shine a light on this critical aspect of recovery, exploring how modern technology like the InBody Body Water Analyzer (InBody BWA2.0S) is revolutionizing its early detection and management.
Why Lymphedema Develops
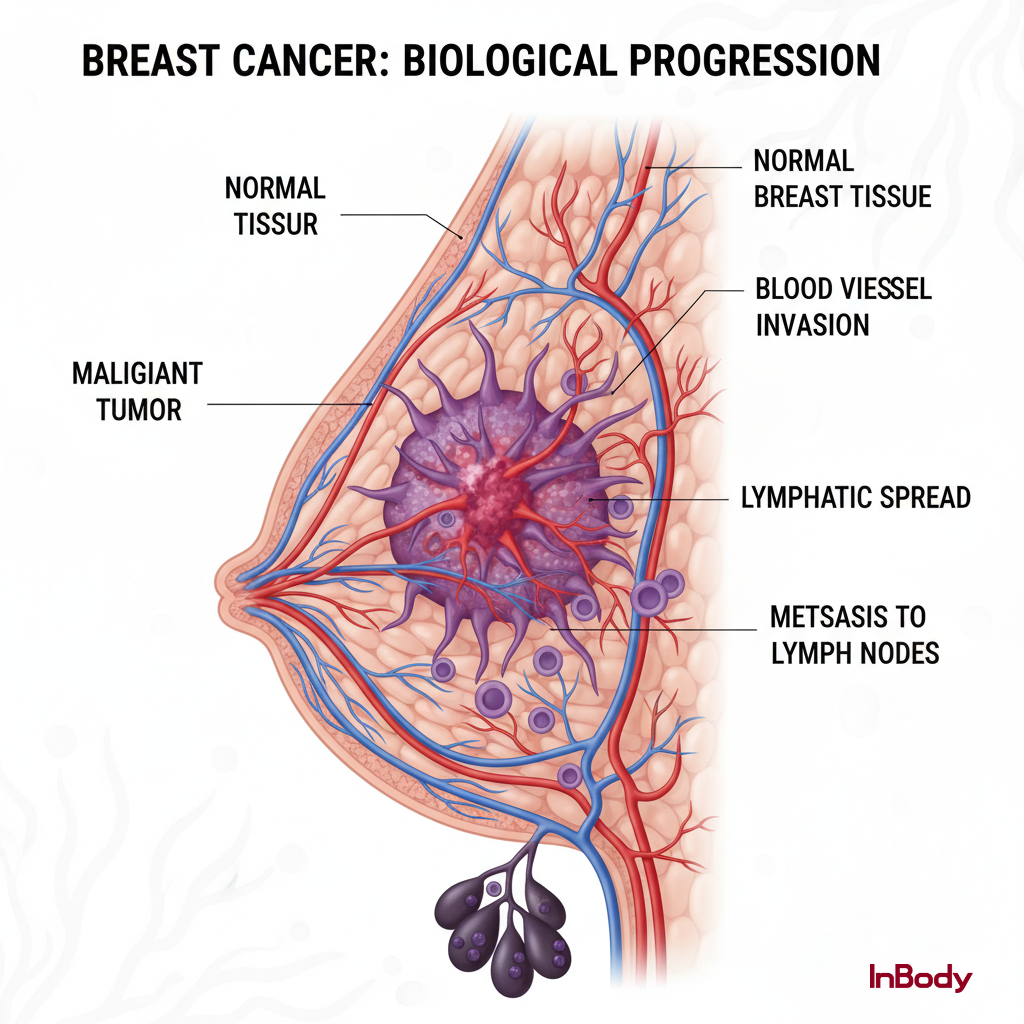
Breast cancer remains the most common cancer among women worldwide, affecting roughly 1 in 8 during their lifetime. Thanks to advances in screening and treatment, survival rates have soared. However, life-saving procedures often come with an inherent risk.
The removal of lymph nodes (a common part of cancer surgery) or the damage to lymphatic vessels from radiation therapy can disrupt the body’s delicate plumbing system. This is the root cause of lymphedema.
What is Lymphedema?
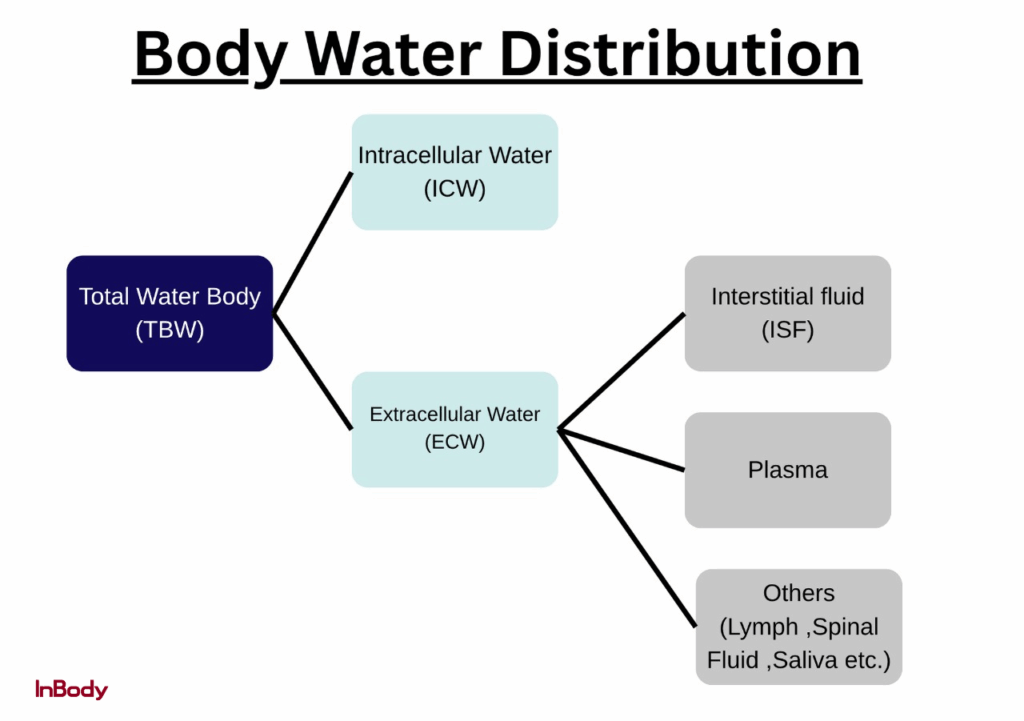
Imagine your body’s circulatory system as a major highway for blood. Running alongside it is the lymphatic system, a specialized drainage network that functions like a slow-moving sanitation crew. Its primary role is to collect interstitial fluid, the protein- and nutrient-rich fluid that bathes tissues, carrying waste products, water, and immune cells and filter it as lymph before returning it to the bloodstream. By doing so, the lymphatic system maintains tissue fluid balance, prevents edema, and supports immune surveillance.
Lymphedema is a chronic condition that occurs when this drainage system is compromised—think of a blocked sewer line. Because the fluid can’t be cleared, it accumulates, leading to persistent swelling, a feeling of heaviness or tightness, and sometimes pain, most commonly in the arm, hand, or chest on the side of the surgery.
The Mechanism: When the Drainage Fails
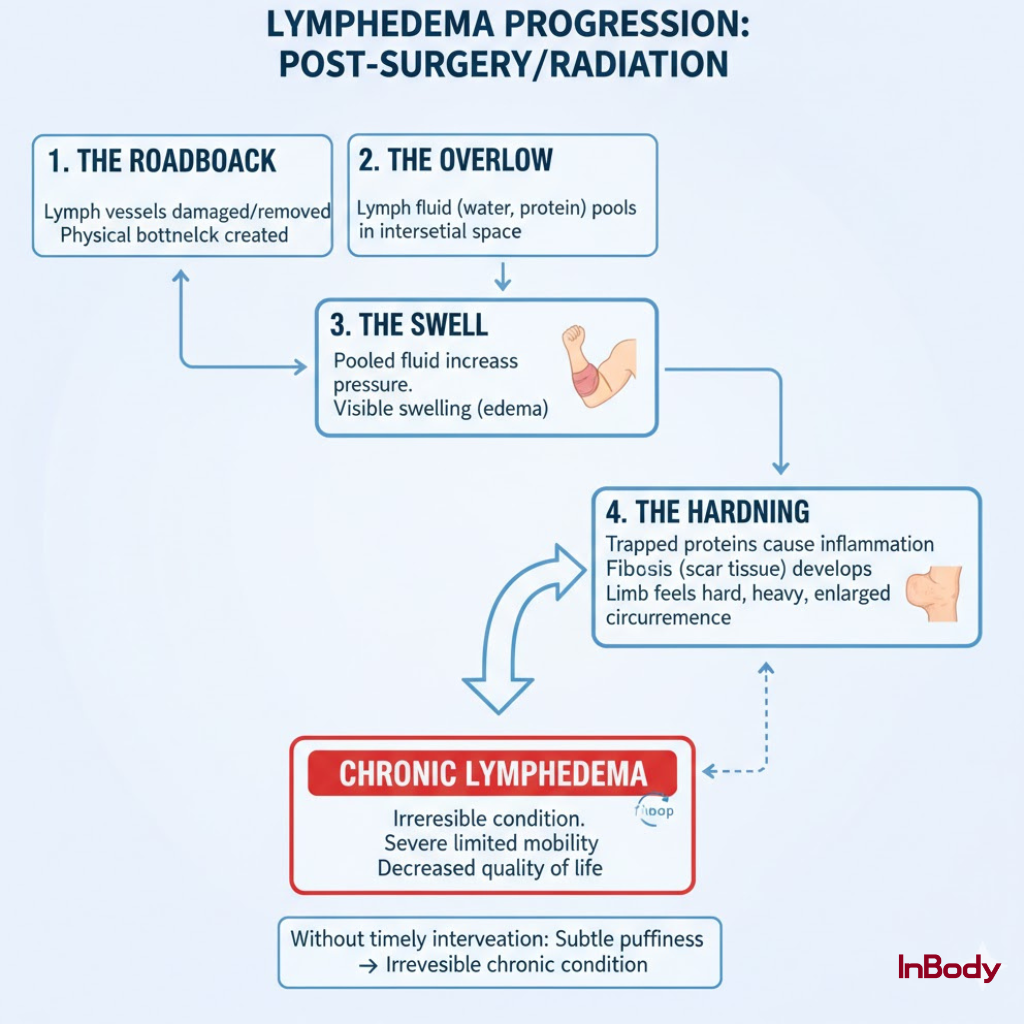
When the lymphatic system is healthy, it is an efficient filter and recycler. Post-surgery or post-radiation, the mechanism is fundamentally broken:
- The Roadblock: Lymph vessels are surgically removed or damaged, creating a physical bottleneck in the fluid’s return path.
- The Overflow: Lymph fluid, especially the water and protein components begins to pool in the interstitial space (the area outside the cells).
- The Swell: This pooling fluid increases pressure, leading to the noticeable swelling.
- The Hardening: Over time, the trapped proteins trigger an inflammatory response. The tissue begins to lay down fibrous, scar-like material (fibrosis), causing the limb to feel hard, heavy, and sometimes dramatically increase in circumference.
Without timely intervention, what starts as subtle, intermittent puffiness can progress to an irreversible, chronic condition that severely limits mobility and quality of life.
The Silent Threat: Why Early Detection is Crucial
The biggest challenge in managing lymphedema is its stealth.
In the early stages, the swelling is often too subtle for a patient or even a clinician to visually spot. Traditional monitoring methods, like simply measuring the limb’s circumference with a tape measure, often only detect the condition after the fluid accumulation has become significant and potentially more difficult to reverse.
This is where a modern, scientific approach is changing the game: Bioelectrical Impedance Analysis (BIA). BIA provides a precise, non-invasive “scan” of where fluid is held in the body, long before it’s visible to the naked eye.
The Water Map: How InBody BWA2.0S Fights Lymphedema
The InBody BWA2.0S is a powerful medical tool that moves beyond standard body composition to focus specifically on the distribution of water. It serves as an essential surveillance tool for lymphedema.
1. Segmental Water Analysis: Pinpointing the Problem
Lymphedema is a regional problem. Swelling doesn’t happen equally across the body, but in a specific limb or area. The InBody BWA2.0S addresses this by performing a Segmental Water Analysis, effectively dividing the body into five distinct ‘water tanks’: the right arm, left arm, trunk, right leg, and left leg.
It breaks down the fluid into two key compartments:
- Intracellular Water (ICW): Fluid inside the cells (where it should be).
- Extracellular Water (ECW): Fluid outside the cells (where lymph fluid pools).
By comparing the Extracellular Water to Total Body Water ratio (ECW/TBW ratio) between the affected and unaffected limb, clinicians gain an objective, quantitative measure. An elevated ratio in one arm, even a tiny one, is the early warning sign of fluid accumulation that signals the onset of lymphedema.
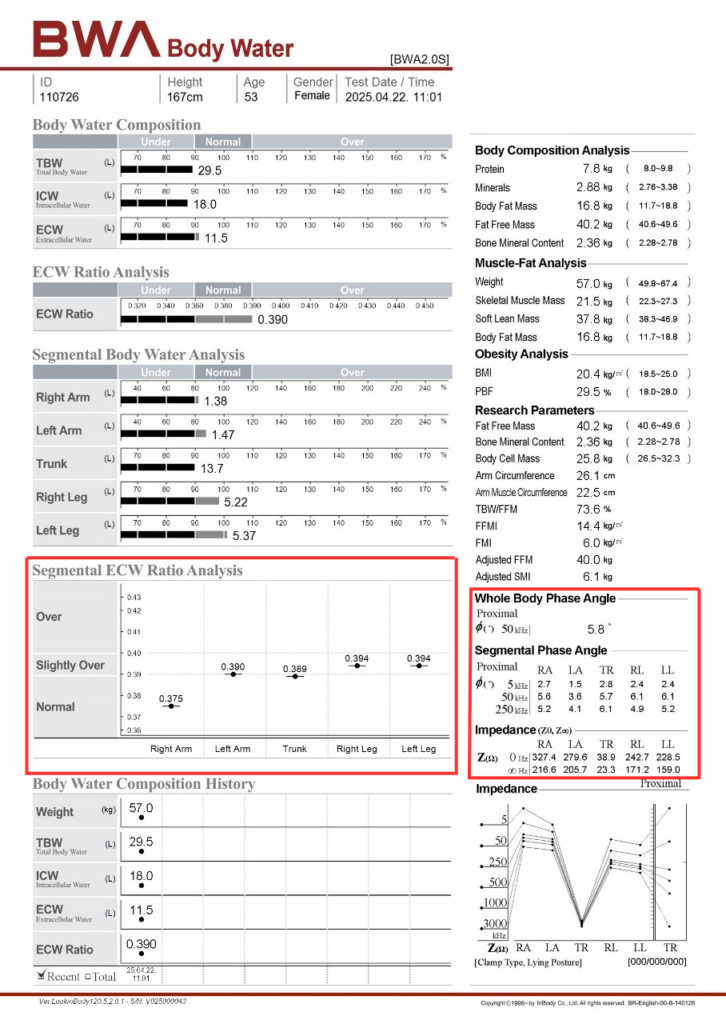
Key Observation from the Resultsheet-
- There is a clear asymmetry between the right and left arms, with the right arm showing a lower water volume (0.375) compared to the left arm (0.390). The difference between them is 0.015, which exceeds the expected physiological variation range of 0.006. This higher-than-normal variation may indicate localized fluid imbalance, possibly due to mild inflammation, edema, or altered tissue hydration in the left arm.
The phase angle (PA) represents cell membrane integrity and cellular health.
- The phase angle in the right arm (5.6°) is lower compared to the left arm (6.3°), indicating reduced cell membrane integrity and compromised cellular function. The difference of 0.7° exceeds the expected physiological variation limit of 0.6°, suggesting possible localized edema or inflammatory changes in the right arm.
- This further supports localized lymphedema, where cellular health is compromised due to fluid overload and tissue compression.
The InBody BWA2.0S report indicates localized lymphedema in the right arm, consistent with post-breast cancer treatment changes.
Evidence includes:
- Elevated ECW/TBW ratio in the affected limb
- Reduced phase angle in the same region
- Normal trunk and lower limb readings, ruling out systemic fluid overload
Recommendations:
- Regular monitoring using InBody BWA2.0S to track segmental ECW/TBW changes.
- Helps in monitoring and improving phase angle.
- Compression therapy if swelling persists or increases.
- Hydration and balanced nutrition to support cellular recovery.
- Helps physiotherapists in early follow-up scans to assess progress in ECW normalization.
2. Quantitative and Trackable: The Power of Data
3. Research Reference
Summary:
In this research, the InBody device was utilized to assess body composition and detect early fluid changes associated with subclinical lymphedema in the upper limbs. Using bioelectrical impedance analysis (BIA), the study compared extracellular water ratios and segmental impedance values between the affected and unaffected arms. The results demonstrated that the InBody can effectively identify early fluid accumulation and tissue changes before visible swelling occurs, making it a valuable tool for early screening and prevention of lymphedema progression.
The entire test is non-invasive, takes less than two minutes, and uses no needles or radiation. It’s an effortless addition to a follow-up visit, promoting consistent, ongoing monitoring without discomfort, empowering patients to take proactive control of their recovery
The Takeaway: Empowering Survivors
Lymphedema is a challenging side effect of life-saving breast cancer treatment, but it is not an inevitable sentence. With early awareness and the use of sophisticated tools like the InBody BWA2.0S, this condition can be detected and managed effectively.
This Breast Cancer Awareness Month, let’s commit to not only celebrating the fight against cancer but also to empowering survivors with the tools and knowledge they need to navigate the long journey of recovery and live healthier, more confident lives.
FAQ
What are the early signs of lymphedema I should look out for?
Early symptoms include a feeling of heaviness, tightness, tingling, or mild swelling in one arm, hand, or chest area. Jewelry or clothes may start to feel tighter on one side. Even subtle changes should prompt a check-up and a body water analysis scan for confirmation.
How does the InBody BWA help detect lymphedema early?
The InBody Body Water Analyzer (BWA) uses advanced bioelectrical impedance technology to measure fluid balance in different body segments. It compares the extracellular water (ECW) to total body water (TBW) ratio in both arms, allowing clinicians to detect even slight fluid buildup—often before it becomes visible.
How reliable is the ECW/TBW ratio in identifying lymphedema?
Extremely reliable. A higher extracellular water to total body water (ECW/TBW) ratio in one limb compared to the other is a validated indicator of localized fluid retention. Clinicians use it as an objective and quantitative measure for both diagnosis and follow-up progress.
How often should a breast cancer survivor get an InBody BWA scan?
It’s recommended to get a baseline scan before or right after surgery, followed by regular scans every 3–6 months, or sooner if swelling, tightness, or discomfort occurs. Consistent tracking helps identify early fluid shifts before lymphedema becomes chronic.
Is lymphedema reversible once it develops?
In its early stages, lymphedema can be managed effectively and sometimes reversed with timely therapy. However, once fibrosis (tissue hardening) sets in, it becomes a chronic condition that requires ongoing management. Routine InBody scans and consistent treatment can help control symptoms and prevent progression.
References
McLaughlin SA, et al. Considerations for Clinicians in the Diagnosis, Prevention, and Treatment of Breast Cancer-Related Lymphedema: Part 1. Ann Surg Oncol. 2017.
https://pubmed.ncbi.nlm.nih.gov/28766232/ PubMed
DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013.
https://pubmed.ncbi.nlm.nih.gov/23540561/ PubMed
[Alternate access via The Lancet site] (https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(13)70076-7/abstract) The Lancet+1
He L, et al. Lymphedema in survivors of breast cancer (Review). Oncol Lett. 2020.
https://www.spandidos-publications.com/10.3892/ol.2020.11307 Spandidos Publications
Breast cancer-related lymphedema: risk factors, precautionary measures and management (PMC article).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6107585/ PMC
Overview of Lymphedema for Physicians and Other Health Care Professionals. Mayo Clinic Proceedings. 2022.
https://www.mayoclinicproceedings.org/article/S0025-6196(20)30033-1/abstract

