Understanding Lymphoma
When people hear the word lymphoma, they often think only of cancer cells multiplying in the body.
While modern therapies like chemotherapy, radiation, and immunotherapy have improved survival, they also bring side effects that affect muscle, water balance, and cellular health. Recognizing and managing these hidden changes can make the difference between treatment challenges and recovery success.
Lymphoma has two main types:
| Feature | Hodgkin Lymphoma (HL) | Non-Hodgkin Lymphoma (NHL) |
| Prevalence | Less common (about 10% of cases) | More common (about 90% of cases) |
| Age Group | Often affects young adults (15–35) and older adults | Can occur at any age, more frequent in older adults |
| Key Cells Involved | Presence of Reed–Sternberg cells | No Reed–Sternberg cells |
| Spread Pattern | Typically orderly (from one lymph node group to the next) | Often non-contiguous, can spread randomly |
| Prognosis | Generally better with modern treatment | Varies widely depending on subtype |
Together, they account for a significant share of global cancer cases. With better treatments available today, patient survival is increasing, but the quality of survival is where body composition becomes a crucial factor.

How Lymphoma Treatment Affects the Body
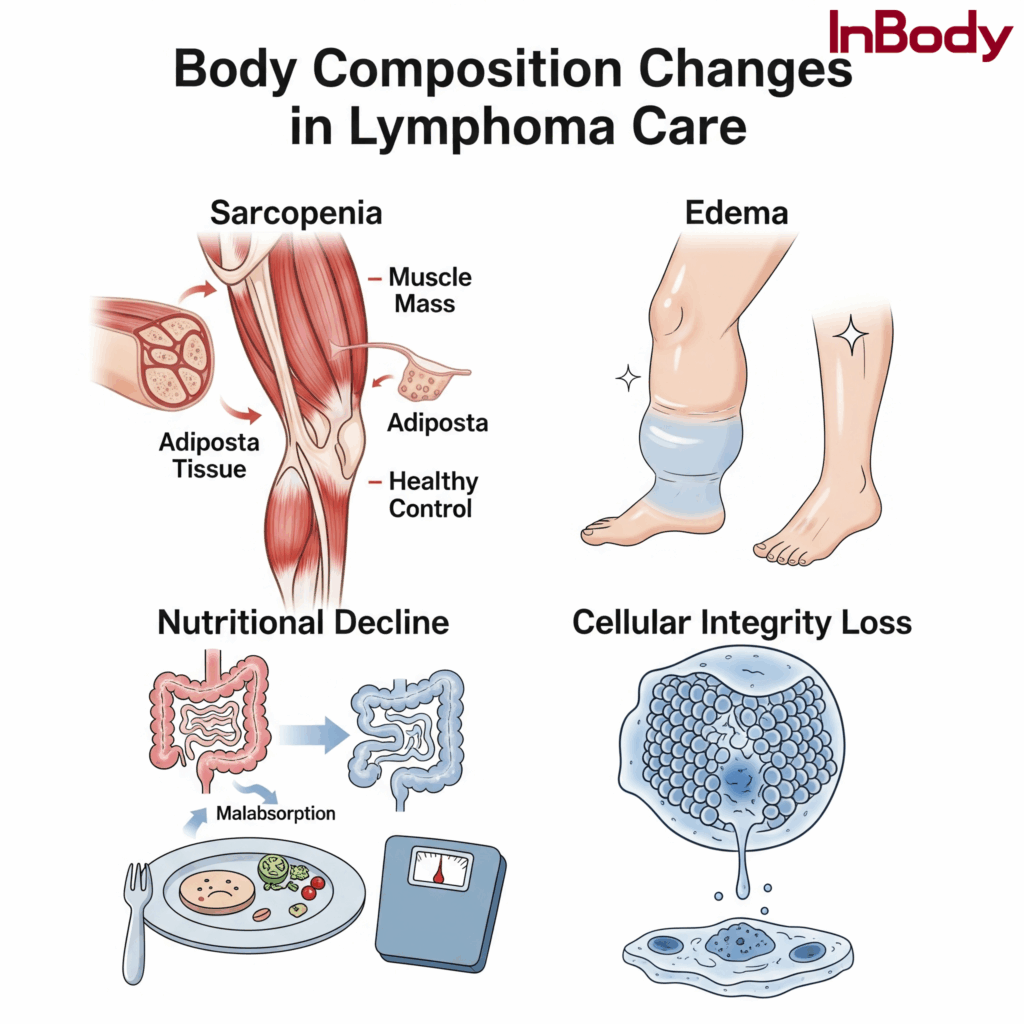
- Muscle Wasting (Sarcopenia & Cachexia)
- Cancer-driven inflammation and reduced physical activity lead to progressive muscle mass loss.
- Cachexia, a syndrome of muscle and fat wasting, is common in advanced lymphoma.
- Sarcopenia worsens treatment outcomes: patients with lower muscle mass have higher chemotherapy toxicity, more complications, and longer hospital stays.
2. Edema & Fluid Imbalances
- Chemotherapy, corticosteroids, and lymph node damage can cause lymphedema and abnormal fluid retention.
- Ascites (fluid buildup in the abdomen) may also occur in advanced cases.
- Traditional measures like body weight or BMI cannot differentiate between fat, muscle, and fluid.
3. Nutritional Decline & Cellular Damage
- Lymphoma treatment often suppresses appetite and causes malabsorption.
- This leads to protein-energy malnutrition, which in turn weakens the immune system.
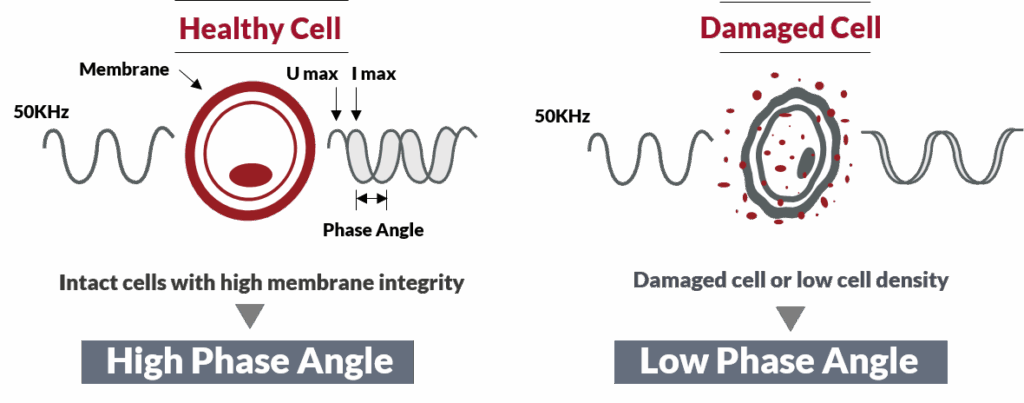
- Cellular integrity declines, which can be tracked through bioelectrical impedance markers like Phase Angle.
Role of Body Composition in Lymphoma Care
Effective cancer care today goes beyond tumor control, it focuses on preserving strength, function, and quality of life.
This is where body composition analysis becomes essential:
• Detecting sarcopenia and cachexia before it’s clinically visible.
• Monitoring fluid retention objectively instead of relying only on symptoms.
• Using Phase Angle as a prognostic indicator of survival and nutritional status.
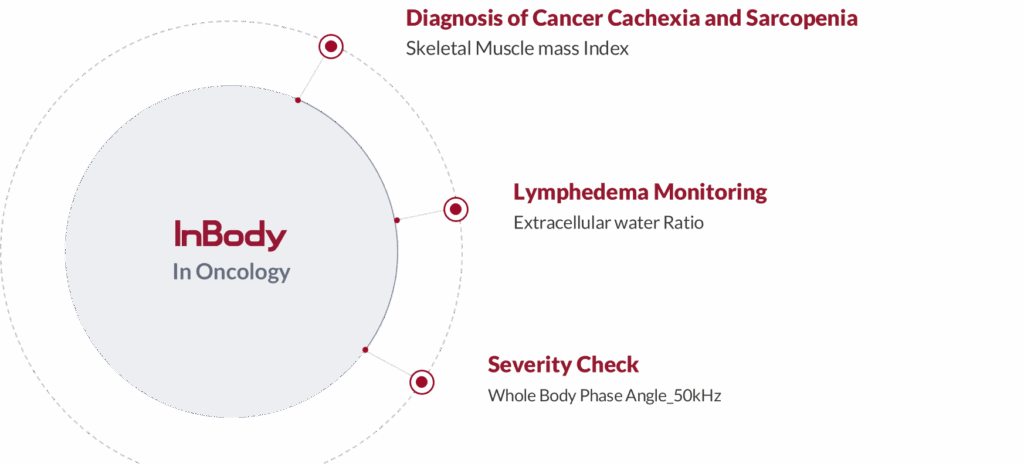
🔹 How the InBody 970S Supports Lymphoma Patients
The InBody 970S is an advanced body composition analyzer that provides deep, clinically relevant insights for both patient care and research, and has been widely used in various clinical studies—for example, in oncology research to assess the relationship between phase angle and cancer prognosis.
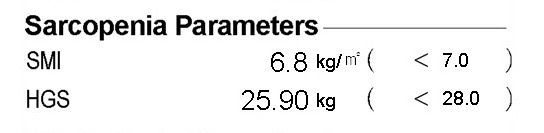
1. Sarcopenia & Cachexia Assessment
- Skeletal Muscle Mass Index (SMI): Identifies muscle loss early, even before it is visible on the outside.
- Segmental Analysis: Shows if muscle wasting is localized (e.g., legs) or systemic.
- Clinical Value: Helps oncologists and dietitians design nutrition and rehabilitation strategies to maintain strength and reduce treatment side effects.
2. Edema & Fluid Balance Monitoring
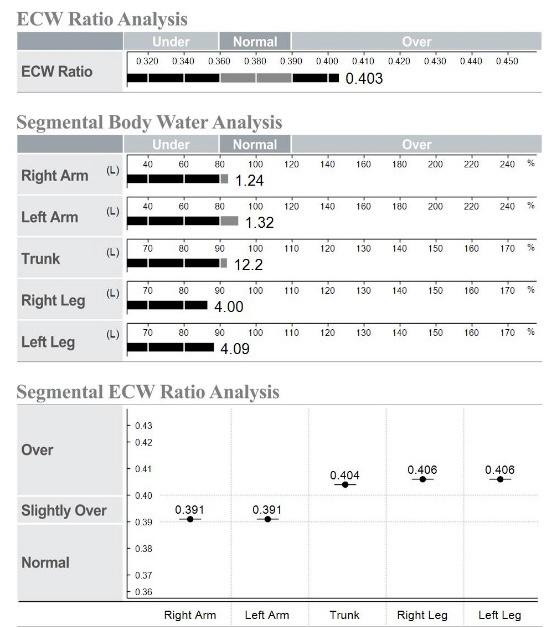
- ECW/TBW Ratio (Extracellular Water to Total Body Water): A reliable indicator of edema and hydration status.
- Segmental ECW Analysis: Detects lymphedema in specific limbs, commonly seen after radiation or lymph node removal.
- Clinical Value: Allows precise monitoring of treatment-induced side effects, guiding fluid management and physical therapy.
3. Phase Angle: Prognostic & Severity Check
- Phase Angle (PhA): Reflects cell membrane integrity and body cell mass.
- Lower PhA: Associated with poor survival, higher treatment toxicity, and malnutrition in lymphoma and other cancers.
- Clinical Value: Oncologists can use Phase Angle trends to predict prognosis and adjust interventions proactively.
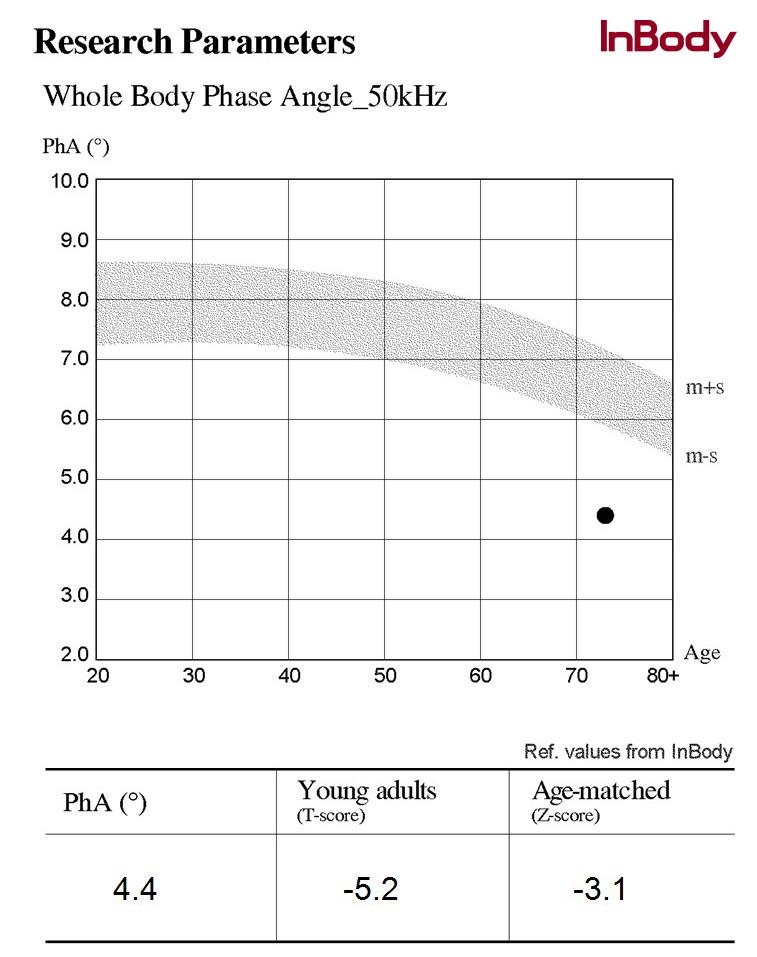
This is the graph of a cancer patient’s InBody report, showing their Phase Angle (PhA) result. The patient’s measured PhA is 4.4°, which lies below the shaded normal range in the graph.
The highlighted (shaded) part represents the reference range, where healthy values are usually expected. A higher phase angle indicates stronger, healthier cells with good nutrition, while a lower phase angle suggests weakened cell membranes and poor nutritional reserves.
In this patient’s case:
- The PhA is much lower than healthy young adults (T-score: -5.2).
- It is also lower than the average of people of the same age (Z-score: -3.1).
This means the patient’s cells are not functioning well, and their nutritional status is compromised. Low phase angle values like this are often found in cancer patients, since the disease and its treatments can damage cells, cause inflammation, and accelerate muscle and nutrition loss.
Why InBody 970s Matter
The InBody 970s uses a 3 MHz high-frequency technology, allowing measurements to penetrate deep into the cells for more precise insights. Unlike basic devices, this premium model can capture subtle changes in cell health, hydration, and nutrition, making it especially valuable in critical conditions like cancer, kidney disease, and severe malnutrition. With its advanced accuracy, it helps clinicians track progress, personalize treatments, and support better patient outcomes.
Improvements in cell membrane and functionality – Phase angle increase
Deterioration cellular integrity and selective permeability- Phase angle decrease
4. A Tool for Research & Awareness
Beyond clinical care, the InBody 970S contributes to research initiatives and awareness programs by:
• Providing objective, repeatable data for oncology studies.
• Supporting clinical trials on nutrition, rehabilitation, and survivorship.
• Highlighting the often-overlooked importance of body composition in cancer outcomes.
Closing Thought
On World Lymphoma Awareness Day, it is crucial to remember that fighting cancer is not only about shrinking tumors, it’s also about maintaining the strength and resilience of the patient.
By integrating advanced body composition tools like the InBody 970S, healthcare providers can:
• Detect sarcopenia and cachexia early,
• Monitor edema and hydration status objectively,
• Use Phase Angle as a guide for prognosis and recovery,
• And ultimately, improve the quality of life for patients battling lymphoma.
Body composition is more than numbers, it’s a roadmap to better outcomes in cancer care.
FAQ
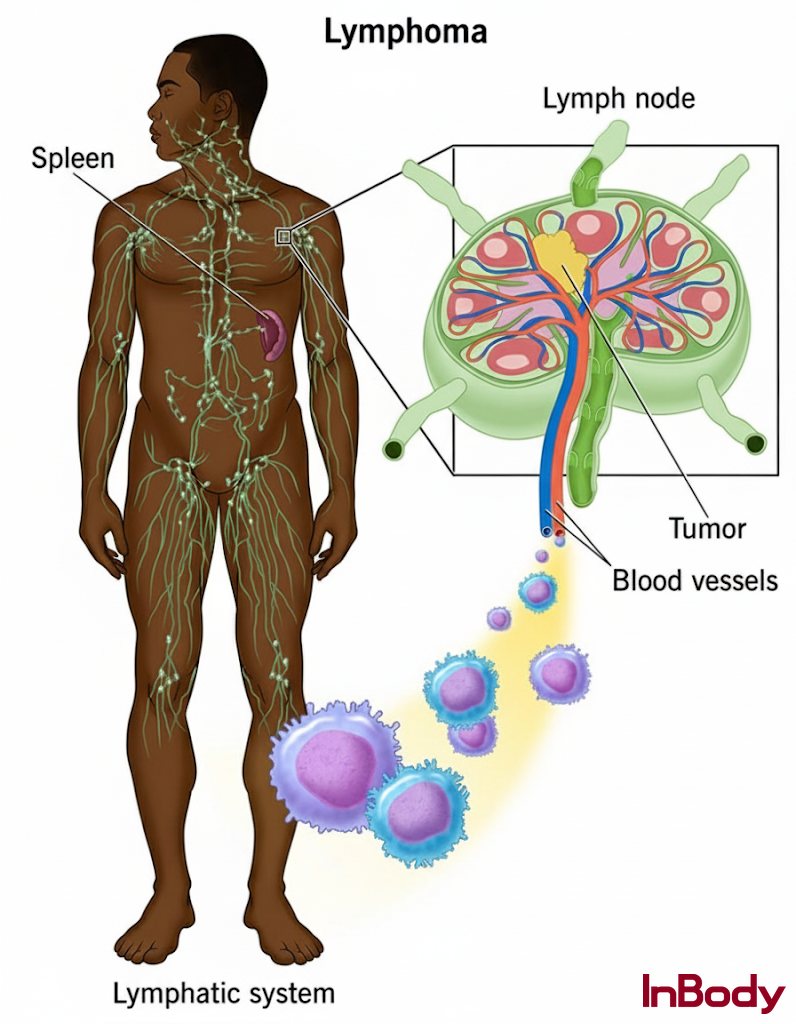
What is lymphoma and how is it different from other cancers?
Lymphoma is a cancer of the lymphatic system, which is part of the body’s immune defense. Unlike solid tumors, lymphoma affects the blood and lymph nodes, spreading through immune pathways.
How does muscle loss (sarcopenia) affect cancer treatment?
Patients with lower muscle mass experience higher chemotherapy toxicity, more complications, and longer hospital stays. Identifying sarcopenia early allows doctors to adjust treatment and add nutrition or exercise interventions.
How does body composition analysis improve quality of life for cancer patients?
By detecting muscle wasting, malnutrition, and fluid imbalance early, healthcare teams can intervene with targeted nutrition, physical therapy, and fluid management. This leads to faster recovery, better energy levels, and improved resilience during treatment.
What role does hydration and fluid balance play in cancer patients?
Chemotherapy, steroids, and lymph node damage can cause abnormal fluid retention or lymphedema. Body composition analysis helps track extracellular water, ensuring proper fluid management during treatment.
What is Phase Angle, and why is it important in cancer patients?
Phase Angle is a bioelectrical marker of cell health and integrity. A lower Phase Angle is linked with poor survival, malnutrition, and higher treatment toxicity in lymphoma patients.
References
1. Yip C, Yong WP, Tai WM, et al. Body composition in cancer: the role of sarcopenia and cachexia in patient outcomes. J Cachexia Sarcopenia Muscle. 2015;6(4):284-293. doi:10.1002/jcsm.12038. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4519815/
2. Guo J, Xu B, Liu S, et al. Skeletal muscle mass index and skeletal muscle density predict chemotherapy toxicity and prognosis in diffuse large B-cell lymphoma. Support Care Cancer. 2021;29:7003-7013. doi:10.1007/s00520-021-06410-2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8025815/
3. Amano K, Matsumoto T, Kaneko S, et al. Prognostic value of phase angle in cancer patients: a systematic review. Nutrients. 2023;15(8):1842. doi:10.3390/nu15081842. https://pubmed.ncbi.nlm.nih.gov/36484944/
4. InBody USA. InBody 970S: Advanced Body Composition Analyzer. InBody USA. Accessed September 18, 2025. https://inbodyusa.com/products/inbody970s
5. Dalla Rovere M, Verzola A, Oliva R, et al. Phase angle and hand grip strength as predictors of 12-month mortality in hematologic cancer patients. Cancers (Basel). 2025;17(5):886. doi:10.3390/cancers17050886. https://www.mdpi.com/2072-6694/17/5/886