Uncovering the Hidden Link Between Lean PCOS and Visceral Fat
“You look healthy, fit, and slim, but inside, your body could be fighting a hidden battle you can’t see.”
Many women believe that being slim protects them from health issues like PCOS. But the reality is shocking: lean women can have PCOS too, often silently struggling with insulin resistance, hormonal imbalances, and hidden fat around their organs. This invisible danger, known as visceral fat, can silently sabotage metabolism, fertility, and long-term health.
Thankfully, modern tools like the InBody H30 bring this hidden metric into clear view, allowing women to take control of their health before problems escalate.
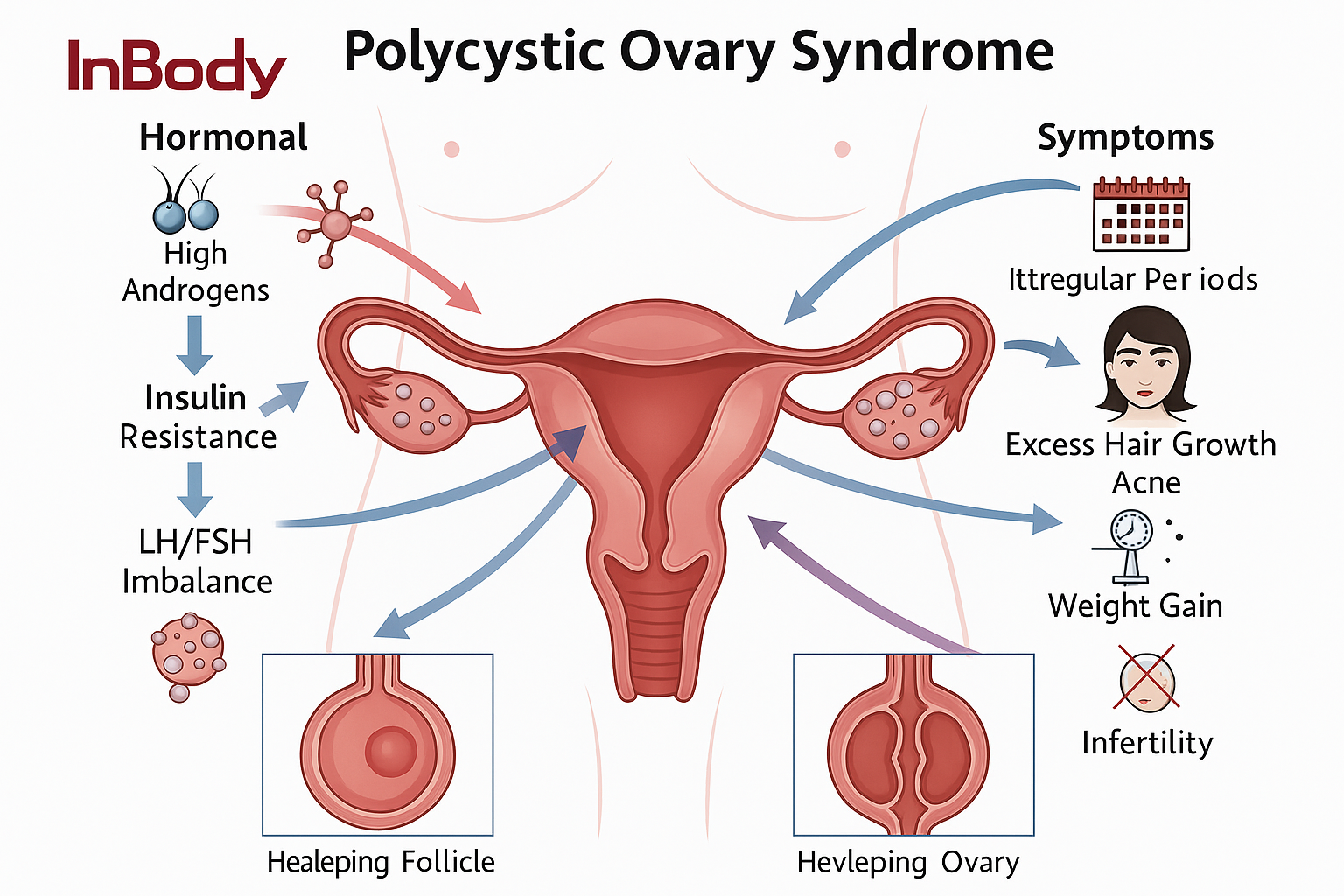
What is Lean PCOS?
PCOS is typically associated with weight gain, acne, irregular periods, and insulin resistance. But not all women with PCOS are overweight. In fact, lean PCOS affects women with a normal BMI, who may look healthy on the outside but face serious internal metabolic challenges.
Key Features of Lean PCOS:
- Irregular or missed periods
- Polycystic ovaries detected on ultrasound
- Hormonal imbalances, particularly elevated androgens
- Insulin resistance without noticeable weight gain
- Fat accumulation in the abdominal region, often visceral fat
This explains why many lean women with PCOS are misdiagnosed or undiagnosed for years. Traditional health checks may show “normal” weight and BMI, but internal fat and metabolic health are not measured on a regular scale.
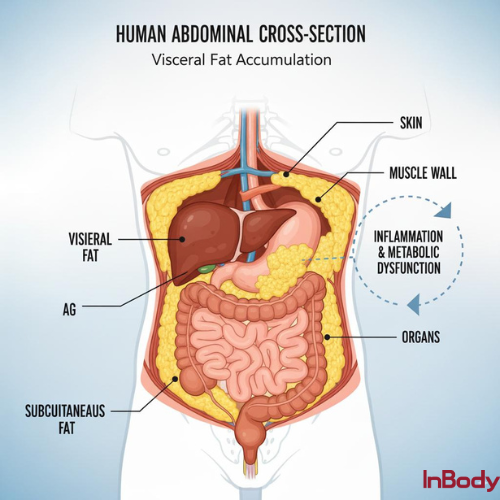
Why Visceral Fat Matters?
Visceral fat is the fat stored deep inside the abdomen, surrounding vital organs such as the liver, pancreas, and intestines. Unlike subcutaneous fat, which lies just under the skin, visceral fat is metabolically active, producing inflammatory chemicals and hormones that can disrupt insulin signaling, metabolism, and reproductive hormones.
Even women who appear slim can have high visceral fat levels, putting them at risk for:
- Insulin resistance → leads to blood sugar spikes and diabetes risk
- Hormonal imbalances → worsens androgen dominance and PCOS symptoms
- Fertility challenges → disrupts ovulation and menstrual cycles
- Long-term health risks → cardiovascular disease, metabolic syndrome
Visceral fat is the hidden enemy of lean PCOS, and tracking it is essential for early detection and management.
Mechanism: How Visceral Fat Drives Lean PCOS
| Step | Mechanism | Outcome in Lean PCOS |
| 1. Hidden Visceral Fat Accumulation | Fat stored around liver, pancreas, intestines | Not visible on BMI/scale but metabolically active |
| 2. Release of Adipokines & Inflammatory Cytokines | ↑ TNF-α, IL-6, resistin | Chronic low-grade inflammation |
| 3. Impaired Insulin Signaling | Inflammation disrupts insulin receptor pathways | Insulin resistance despite normal weight |
| 4. Compensatory Hyperinsulinemia | Pancreas releases excess insulin | Exacerbates ovarian androgen production |
| 5. Hyperandrogenism | ↑ Testosterone, DHEA-S | Acne, hair growth, ovulation dysfunction |
| 6. Ovarian Dysfunction | Altered LH:FSH ratio, disrupted folliculogenesis | Irregular cycles, anovulation, infertility |
| 7. Long-Term Risk | Persisting visceral fat + hormonal imbalance | Type 2 diabetes, metabolic syndrome, CVD |
The Challenge of Diagnosing Lean PCOS
Lean PCOS is tricky to diagnose because BMI alone does not reveal internal fat levels or hormonal imbalances. Many women remain unaware of their condition until symptoms worsen or fertility issues arise. In conditions like PCOS, where hidden visceral fat and hormonal imbalances play a major role, daily monitoring helps track subtle changes that the scale can’t reveal. Regular insights empower women to adjust nutrition, exercise, and lifestyle strategies in real time. This proactive approach makes it easier to manage symptoms, protect fertility, and prevent long-term health risks.
Commonly Overlooked Symptoms:
- Slight weight gain around the abdomen
- Irregular menstrual cycles
- Unexplained fatigue or blood sugar fluctuations
- Acne, hair growth in unusual places, or thinning hair
Because traditional scales and BMI calculations cannot detect visceral fat, a more precise method is needed—this is where InBody H30 comes in.
How InBody H30 Transforms PCOS Management
The InBody H30 is a cutting-edge device for home body composition analysis, giving users a complete picture of their health beyond just weight. Unlike traditional scales, it provides insights into:
- Visceral fat levels
- Body fat percentage
- Muscle mass
- Water content
For women with lean PCOS, the visceral fat reading is a game-changer. Even if your weight is normal, a high visceral fat level can reveal hidden metabolic stress and hormonal imbalance.
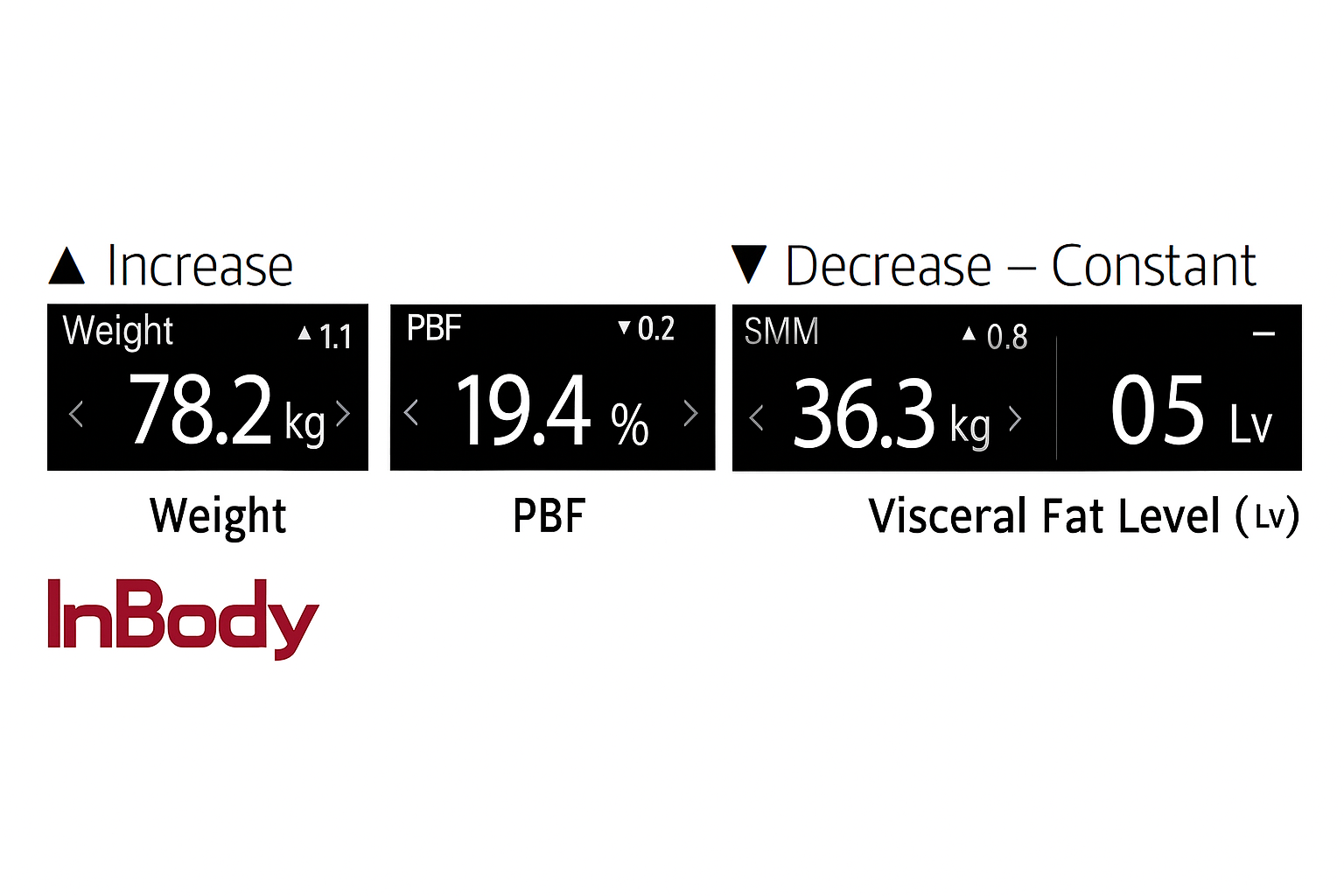
Why Tracking Visceral Fat with InBody H30 Matters:
- Early Detection: Identify internal risks that are invisible on the scale.
- Personalized Health Plans: Tailor diet, exercise, and lifestyle changes based on actual body composition.
- Progress Monitoring: Track improvements over time and see real results.
- Motivation: Numbers make health progress tangible, helping women stick to their wellness routines.
With InBody H30, women with lean PCOS can take proactive steps toward improved hormonal balance, metabolism, and long-term health.
Lifestyle Strategies to Combat Lean PCOS and Visceral Fat
Once visceral fat is identified as a risk factor, targeted lifestyle changes can make a huge difference:
1. Nutrition
- Focus on low-glycemic, anti-inflammatory foods: leafy greens, whole grains, lean proteins, and healthy fats.
- Limit processed foods and sugars to control insulin levels.
- Track meals to avoid hidden triggers for insulin spikes.
2. Exercise
- Combine resistance training with cardio to reduce visceral fat and boost metabolism.
- High-Intensity Interval Training (HIIT) is especially effective for abdominal fat reduction.
- Regular activity improves insulin sensitivity and hormone balance
3. Stress Management
- Chronic stress elevates cortisol, which worsens visceral fat accumulation.
- Incorporate meditation, yoga, or deep breathing exercises to support hormonal health.
4. Sleep
- Aim for 7-9 hours of quality sleep to regulate insulin and cortisol.
5. Medical Support
- Regular monitoring of hormones and insulin levels.
- In some cases, medications like metformin may be recommended by a healthcare professional.
By combining these lifestyle interventions with InBody H30 monitoring, women can see measurable improvements in visceral fat and overall health.
Real-Life Impact: Seeing Beyond the Scale
Consider two women with lean PCOS:
- Woman A: Slim, BMI 22, unaware of high visceral fat. She struggles with irregular cycles and fatigue.
- Woman B: Uses InBody H30 at home, discovers high visceral fat, implements diet and exercise changes, and tracks progress. Over months, visceral fat decreases, insulin sensitivity improves, and symptoms reduce significantly.
The lesson is clear: weight alone is not a health indicator. Tools like the InBody H30 allow women to see what truly matters inside their body.
To get precise measurements of hidden fat and better understand your body composition, we recommend using the InBody H30 device. It provides detailed insights into visceral fat, muscle mass, and other key health metrics, empowering you to take control of your PCOS management.
For more detailed information about the device please visit- https://inbody.in/product/h30.php
Disclaimer: This blog is intended for educational purposes only and shares general tips on lifestyle changes for managing PCOS. It should not be taken as medical advice. If you have persistent symptoms, complications, or serious health concerns, please consult a qualified healthcare professional for proper diagnosis and treatment.
FAQ
Why is visceral fat dangerous if it’s not visible?
Unlike subcutaneous fat (under the skin), visceral fat surrounds organs like the liver and pancreas. It is metabolically active, releasing inflammatory chemicals that disrupt insulin sensitivity and hormones. Even if you look slim, high visceral fat increases risks for diabetes, infertility, and cardiovascular disease.
How often should I track visceral fat with InBody H30?
Most women benefit from checking every 4–6 weeks. This allows you to see trends, monitor the impact of diet and exercise, and make timely adjustments before symptoms or risks escalate.
Is body weight a reliable indicator of health for women with PCOS?
No. A woman can look slim on the outside but still carry harmful visceral fat and metabolic risks inside. Body composition analysis provides a more accurate picture of health than weight or BMI alone.
How does stress impact Lean PCOS and visceral fat?
Chronic stress raises cortisol, a hormone that promotes fat storage in the abdominal area. This can worsen visceral fat buildup, insulin resistance, and hormonal imbalances. Stress management practices like yoga, meditation, or journaling are especially important for women with lean PCOS.
References
- Amisi, C. A., Tchankou, C., Omole, J., & Alloh, F. T. (2022). Markers of insulin resistance in polycystic ovary syndrome. Frontiers in Endocrinology, 13, 867875. https://doi.org/10.3389/fendo.2022.867875
- Jena, D., Sahoo, J., Gopalakrishnan, S., Behera, S., & Behera, P. (2018). Study of visceral and subcutaneous abdominal fat in polycystic ovarian syndrome. Journal of Human Reproductive Sciences, 11(3), 253–258. https://doi.org/10.4103/jhrs.JHRS_70_17
- Barrea, L., Arnone, A., Annunziata, G., Muscogiuri, G., Laudisio, D., Salzano, C., Pugliese, G., Colao, A., & Savastano, S. (2021). Adherence to the Mediterranean diet, dietary patterns and body composition in women with polycystic ovary syndrome (PCOS). Journal of Translational Medicine, 19, 372. https://doi.org/10.1186/s12967-021-03078-w
- Arpaci, D., Gürkan Tocoğlu, A., Yılmaz, S., Ergün, H., Tamer, A., & Ergün, H. (2015). The relationship between epicardial fat tissue thickness and visceral adipose tissue in lean patients with polycystic ovary syndrome. Journal of Ovarian Research, 8, 71. https://doi.org/10.1186/s13048-015-0197-4
- Atakul, T. (2020). Polycystic ovary syndrome in overweight and normal weight women: The relationships with inflammatory markers. Bosphorus Medical Bulletin, 5(3), 124–130. https://doi.org/10.4274/BMB.galenos.2020.03.07

