Can Obesity Rewire Growing Minds?
Surprising Data on Obesity and Mental Health in Childhood obesity is more than a physical health concern it deeply affects mental wellbeing. A prospective study tracking children aged 8-12 into adolescence found those with obesity were over seven times more likely to develop mental health disorders than their peers of normal weight. These children displayed significantly elevated anxiety, depressive symptoms, and deterioration of body esteem over time.
New data presented at the European Congress on Obesity examined over 3,300 teens and discovered those with abdominal obesity had enlarged hippocampus and amygdala regions in the brain areas crucial to memory, learning, and emotion regulation thereby increasing the risk of cognitive and emotional issues later in life.
These alarming findings underscore why childhood obesity today should be seen as an urgent mental as well as physical health challenge.
Not only does childhood obesity make children feel heavier but it also alters the structure of their brains making them more vulnerable to anxiety, depression, and emotional dysregulation. However not all excess weight has the same negative effects on mental health. That’s where precise body composition analysis becomes indispensable it helps distinguish whether a child’s higher body weight stems from visceral fat the kind most closely linked to mental health risk or from lean muscle mass which can actually confer emotional resilience.

Why Understanding Body Composition Matters More than Just Weight?
The precision necessary to distinguish between water mass, muscle mass, and fat mass is lacking in conventional methods like the Body Mass Index (BMI). This limitation can obscure how obesity truly impacts a child’s health and mental state.
Precise body composition analysis breaks this barrier. Using technologies such as bioelectrical impedance analysis (BIA) deployed by InBody devices healthcare and fitness professionals get a detailed view of-
- Total body fat percentage
- Visceral fat (fat around internal organs, which poses greater health risks)
- Lean muscle mass
- Hydration levels
For children this detailed breakdown is critical. In addition to weight visceral fat strongly correlates with negative metabolic and psychological outcomes. On the other hands it appears that physical fitness and lean muscle protect young people from anxiety and depression.
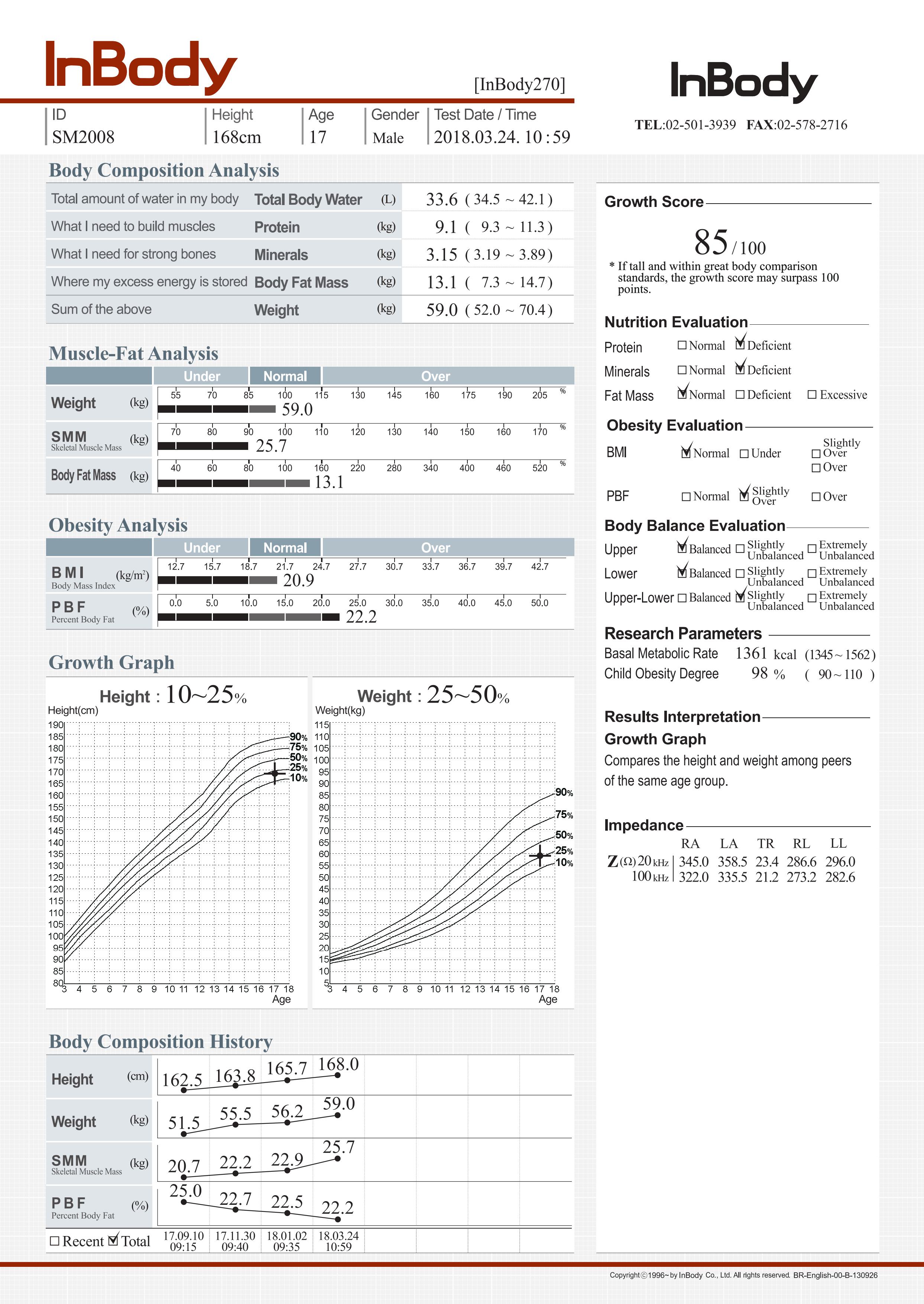
This InBody children result sheet highlights the importance of looking beyond weight alone when assessing obesity. Although the 17-year-old male weighs 59 kg with a BMI of 20.9 (within the normal range), the detailed analysis shows how muscle mass, fat mass, and body balance contribute to overall health. His body fat percentage (22.2%) is slightly on the higher side but still within acceptable limits, while muscle mass has steadily improved over time. The growth score of 85/100 reflects good development, but his height is on the lower percentile compared to peers, reminding us that growth patterns vary individually. Also the growth graph implies that the height is below average (10-25th), while weight is average (25-50th), showing a slight imbalance in growth.
This case emphasizes that obesity is not just about being “overweight” on the scale it’s about the balance of fat and muscle, healthy nutrition, and lifestyle.
Translating Data into Better Mental Health Outcomes for Children
Clinicians and fitness professionals can use advanced body composition analyzers like InBody to:
• Monitor visceral fat and lean mass to identify early mental health challenges.
• Guide personalized interventions using objective data, motivating children and families through progress tracking
• Support holistic health programs that integrate physical fitness promotion as a mental health strategy
In point of fact, the in-depth Children’s Interpretation Sheet from InBody India provides a straightforward, expert overview that assists parents and practitioners in comprehending the significance of parameters such as muscle mass, fat distribution, and hydration to a child’s physical and mental overall wellness.

Conclusion: Advancing Child Health Through Precision and Compassion
In addition to conventional methods precise tools and a holistic perspective are required to address childhood obesity and its profound effects on mental health. InBody’s advanced body composition analysis combined with its intuitive Children’s Result Sheet, empowers healthcare professionals, fitness experts, and families with the knowledge and insights needed to intervene early and effectively.
India’s children deserve the best technology and care to lead them toward healthier, happier futures in a world that is changing quickly and facing more and more challenges to lifestyle choices. We can break the cycle of childhood obesity and its effects on mental health by working together to innovate raise awareness and provide compassionate support. By doing so we can cultivate resilient generations that thrive in both their bodies and minds.
- FAQ
Can obesity actually change the brain?
Yes, and this is surprising! Research presented at the European Congress on Obesity showed that teens with abdominal obesity had enlarged hippocampus and amygdala—areas linked to memory, learning, and emotion regulation. That means obesity can literally shape the brain in ways that impact both mental health and cognition.
How often should children get a body composition check?
Ideally, every 3–6 months. This helps parents and doctors spot early trends, adjust nutrition and exercise, and celebrate positive changes like muscle gain or healthier fat balance.
What are the symptoms of childhood obesity?
According to science, symptoms of childhood obesity include excess body fat (especially around the stomach and face), a BMI above the 95th percentile for age, tiredness or breathlessness during activity, and sometimes skin changes like dark patches or stretch marks. Children may also show low self-esteem or sleep problems, which are important early warning signs.
At what age can children undergo a Body Composition Analysis (BCA) test?
Children can usually take a BCA test from around 6 years of age, when growth and hydration levels are more stable for accurate results. Some devices may allow testing earlier, but interpretation is most reliable after age 6. This helps track healthy growth, body fat, and muscle balance in developing years.
References
1. Beltrán-Garrayo L. Examining associations between childhood obesity and mental health disorders: A prospective study. Psychiatry Research. 2023 Jun 29;322:115154. Available from: https://www.sciencedirect.com/science/article/pii/S0165178123002469
2. Castro JAC, Nunes HEG, Silva DAS. Prevalence of abdominal obesity in adolescents: Association between sociodemographic factors and lifestyle. Revista Paulista de Pediatria. 2016 Sep;34(3):343–351. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC5178121/
3.Papadimitriou K, Mentzelou M, Papadopoulou SK, et al. Childhood obesity and overweight are associated with higher risk of depression and anxiety: A cross-sectional study in children aged 6–9 years. Life (Basel). 2025 Jun;15(6):968. Available from: https://doi.org/10.3390/life15060968
4. Lindberg L, Hagman E, Danielsson P, et al. Anxiety and depression in children and adolescents with obesity: a nationwide study in Sweden. BMC Medicine. 2020 Mar 3;18(1):30. Available from: https://doi.org/10.1186/s12916-020-1498-z
5. Kang NR, Kwack YS, et al. An Update on Mental Health Problems and Cognitive Behavioral Therapy in Pediatric Obesity. Pediatric Gastroenterology, Hepatology & Nutrition. 2020 Jan;23(1):15–25. Available from: https://doi.org/10.5223/pghn.2020.23.1.15

