Albumin: Important but Not Enough – The GLIM Shift
Serum albumin is widely used in Indian hospitals and public health programs to assess nutritional status, helping identify patients who may need targeted nutrition therapy in conditions like chronic kidney disease, cancer, or post-surgical recovery. However, albumin levels can be misleading often lowered by inflammation regardless of nutritional reserves making it more of an inflammation marker (a “negative acute-phase reactant”) than a true indicator of nutrition. Recognizing this limitation, four major societies ASPEN, ESPEN, FELANPE, and PENSA introduced the Global Leadership Initiative on Malnutrition (GLIM) criteria in 2018, which emphasize measuring muscle mass alongside biochemical markers. Japan and France regularly check muscle mass as part of nutrition care. In India, combining muscle mass checks with serum albumin can give a clearer view of a patient’s health. Muscle mass matters because it shows how strong a person is, how well they can recover, and how healthy they are overall.
What Does GLIM Guidance Mean for Diagnosing Malnutrition?
The Global Leadership Initiative on Malnutrition, better known as GLIM, came into existence in 2016. It was the result of a joint effort between four major international clinical nutrition societies ESPEN, ASPEN, FELANPE, and PENSA. The goal was simple but ambitious: create a single, worldwide standard for defining and diagnosing malnutrition.
Before this, nutritional assessment often depended on a clinician’s personal judgment. Different countries used different benchmarks, which made research comparisons tricky and slowed down any coordinated global strategy. GLIM was designed to cut through this problem, and over the years, it has caught on. By February 2025, PubMed had listed more than 460 studies referencing the framework.
GLIM works in three main stages. First, there’s risk screening spotting people who might be at risk. This can be done with any validated tool, such as the MUST or NRS-2002. If the person is flagged as “at risk,” the next step is a full diagnostic assessment, which looks at five specific criteria. These are split into two groups: three are phenotypic (relating to body measurements and composition) and two are etiologic (relating to underlying causes). To diagnose malnutrition, you need at least one from each category.
Finally, there’s severity grading, which is based only on the phenotypic measures. This last step is important because it not only confirms the problem but also helps guide how urgently and aggressively it should be treated.
HOW TO USE THE GLIM FRAMEWORK

- Why Measuring Muscle Mass Using GLIM Is Often Challenging
When the GLIM criteria were first introduced, they gave a strong overall framework for diagnosing malnutrition. But one thing they didn’t really get into was the nitty-gritty of how to actually measure muscle mass or what numbers to use for defining “low muscle mass.”
That gap was addressed in 2022, when new guidance came out with much more practical detail. This update didn’t change the core principles but clarified how to assess muscle mass and suggested reference cutoffs depending on the method you use.
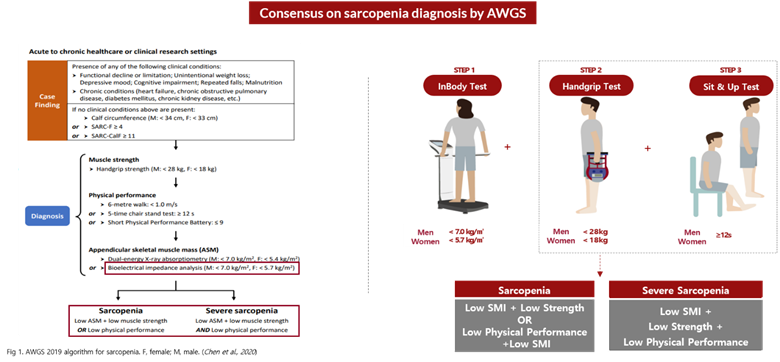
Across the board, skeletal muscle mass is considered the best standard for this kind of assessment. Common ways to measure it include CT scans, DXA scans, and BIA devices. Each tool works differently, so it’s not a one-size-fits-all situation the cutoff values need to take into account things like a person’s age, sex, ethnicity, and whether they’re dealing with an illness.
As for deciding where to draw the line for “low muscle mass,” the update recommends borrowing from existing sarcopenia guidelines like those from the European or Asian working groups and even adapting concepts from osteoporosis scoring systems (T-scores and Z-scores) to keep things consistent and comparable.
There’s a caveat, though. None of these tools not CT, DXA, or BIA directly measure skeletal muscle. They all work indirectly, which means that in cases like obesity or fluid retention, the numbers might look better than they actually are because excess body water can throw off the readings.

- FAQ
What are the GLIM criteria for malnutrition?
The Global Leadership Initiative on Malnutrition (GLIM) introduced an approach for malnutrition diagnosis in 2019 comprised of screening followed by assessment of three phenotypic criteria: weight loss, low BMI, and low muscle mass, and two etiologic criteria: reduced food intake/assimilation, and inflammation/disease.
Is albumin a good indicator of malnutrition?
Is albumin a good indicator of malnutrition?
How does malnutrition affect muscle mass?
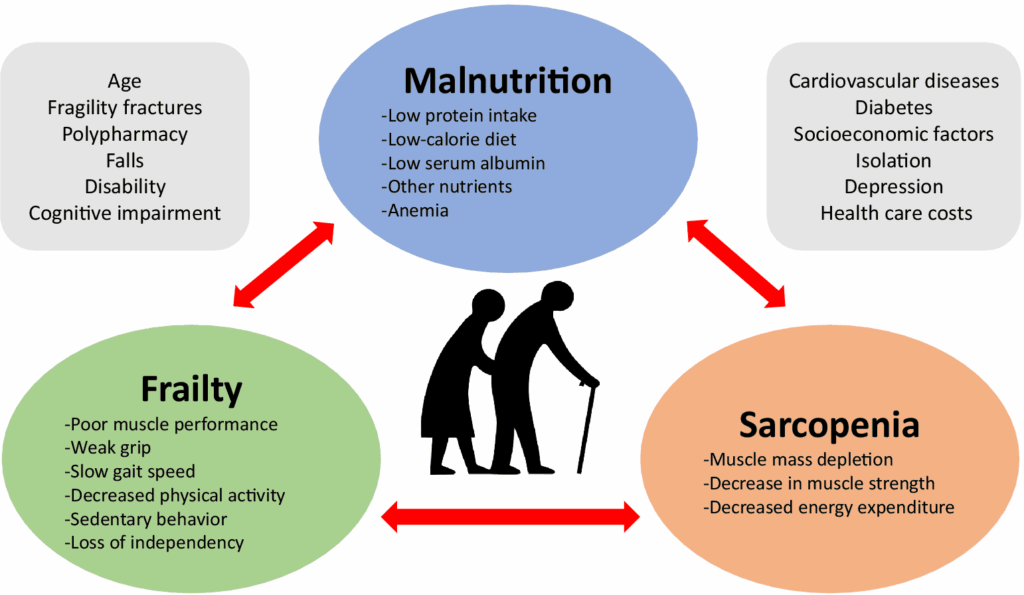
Interestingly, malnutrition seems to be related to muscle health decline and may contribute to the development of sarcopenia [14,15,16] and aggravate the age-associated loss of muscle mass, muscle strength and physical performance [17,18].
What are the Glim criteria for critical care?
The GLIM criteria for diagnosing malnutrition include three phenotypic criteria: weight loss, low Body Mass Index (BMI), and reduced muscle mass, and two etiologic criteria: reduced food intake or assimilation and chronic and/or acute inflammation.
What are the four indicators of malnutrition?
Common signs and symptoms of malnutrition include:
reduced ability to perform everyday tasks like showering, getting dressed or cooking.
loss of appetite and lack of interest in food or fluids.
unplanned weight loss – this might cause clothing, rings, watches or dentures to become loose.
tiredness or low energy levels.
How BWA Technology Fills Gaps in GLIM Muscle Mass Assessment
You see, InBody checks muscle mass using something called Bioelectrical Impedance Analysis, or BIA for short. What’s nice about it is that, unlike CT or DXA scans, there’s no radiation involved at all. That makes it safe even if you need to get tested often. The way it works is pretty simple a small, harmless electrical signal passes through your body, and you don’t feel a thing. The whole process is over in minutes, which is why it’s so handy for keeping track of nutrition and muscle health on a regular basis.
InBody’s Body Water Analyzer (BWA) is a top-tier medical device and also built to tackle many of the gaps highlighted in the GLIM guidelines. It offers a detailed set of readings that help healthcare professionals measure muscle mass more accurately and set practical, real-world cutoff points.
The BWA is the first device in the world to use a 3 MHz high-frequency current also a breakthrough that was once hard to achieve. This technology makes it easier to clearly distinguish between extracellular and intracellular water. It also estimates Z₀ and Z∞, two important values that are useful for both clinical work and research. As together, these features help healthcare professionals evaluate fluid overload in patients with edema more accurately and improve muscle mass measurements.
1) How BWA Overcame the Limitations Pointed Out in the GLIM Guidance
In addition, the BWA provides age-specific assessments is based on over 130 million InBody measurements gathered worldwide. These include T-scores, which compare a person’s results to those of healthy young adults, and age-matched Z-scores, which show how results differ from the average for a specific age group.
Because it focuses on analyzing body fluids, the BWA is especially valuable in important medical areas like fluid monitoring, diagnosing sarcopenia, and assessing how well cells are functioning.
2) BWA: A Promising Tool for Sarcopenia Diagnosis
One of the great things about the BWA is how it’s becoming a go-to tool for diagnosing sarcopenia, whether in small clinics or big university hospitals.
In 2021, Korea officially listed sarcopenia as a medical condition. Since then, this segmental multi-frequency BIA tech has proven its worth in clinics. Even though it’s not reimbursed yet, many doctors are using InBody devices to screen for sarcopenia more regularly.
GLIM guidance also reminds us that malnutrition often plays a big role in sarcopenia. So, it suggests keeping an eye on nutrition in patients who have sarcopenia. As this link becomes clearer, more researchers are turning to BWA for body composition analysis it’s fast becoming a trusted tool in this area.
Muscle mass assessment isn’t just something nice to have anymore it’s actually become a must when it comes to diagnosing malnutrition. Experts everywhere agree on that. Nowadays, since healthcare is focusing more on nutrition, understanding a patient’s muscle condition really matters.
When doctors have solid, reliable muscle measurements, they can personalize treatments way better. And that often means patients heal and recover faster.
That’s why it’s so important for clinics and hospitals to keep up with these new developments and use the best ways to check muscle mass methods that are backed by the latest research and guidelines.
References
1. Jensen GL, Cederholm T, Ballesteros-Pomar MD, Blaauw R, Isabel M, Cuerda C, et al. Guidance for assessment of the inflammation etiologic criterion for the GLIM diagnosis of malnutrition: A modified Delphi approach. Journal of Parenteral and Enteral Nutrition. 2024 Jan 15;Available from: https://pubmed.ncbi.nlm.nih.gov/38221842/
2. Jensen GL, Cederholm T, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM Criteria for the Diagnosis of Malnutrition: A Consensus Report From the Global Clinical Nutrition Community. Journal of Parenteral and Enteral Nutrition. 2018 Sep 2;43(1):32–40. Available from: https://pubmed.ncbi.nlm.nih.gov/30181091/
3.Jensen GL, Cederholm T, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM consensus approach to diagnosis of malnutrition: A 5-year update. JPEN J Parenter Enteral Nutr. 2025;49(1):5–19. Available from: https://aspenjournals.onlinelibrary.wiley.com/doi/10.1002/jpen.2756
4. Compher C, Cederholm T, Correia MITD, Gonzalez MC, Higashiguch T, Shi HP, et al. Guidance for assessment of the muscle mass phenotypic criterion for the Global Leadership Initiative on Malnutrition diagnosis of malnutrition. JPEN Journal of parenteral and enteral nutrition 2022 Apr 19;48(1). Available from: https://pubmed.ncbi.nlm.nih.gov/35437785/
5. Baek JY, Jung HW, Kim KM, Kim M, Park CY, Lee KP, et al. Korean Working Group on Sarcopenia Guideline: Expert Consensus on Sarcopenia Screening and Diagnosis by the Korean Society of Sarcopenia, the Korean Society for Bone and Mineral Research, and the Korean Geriatrics Society. Annals of Geriatric Medicine and Research 2023 27(1):9–21. Available from: https://pubmed.ncbi.nlm.nih.gov/36958807/